The main valvular heart diseases (VHDs), rheumatic heart diseases affect around 41 million people worldwide. VHDs can reduce the quality of life, physical functionality and sometimes cause sudden death.
The current golden standard clinical intervention for VHDs is replacing the diseased valve with mechanical or bioprosthetic valves. But these options are accompanied by severe complications such as blood clot formation, calcification, severe inflammation, limited durability, need for lifelong anticoagulation therapy, and no somatic tissue growth over time.
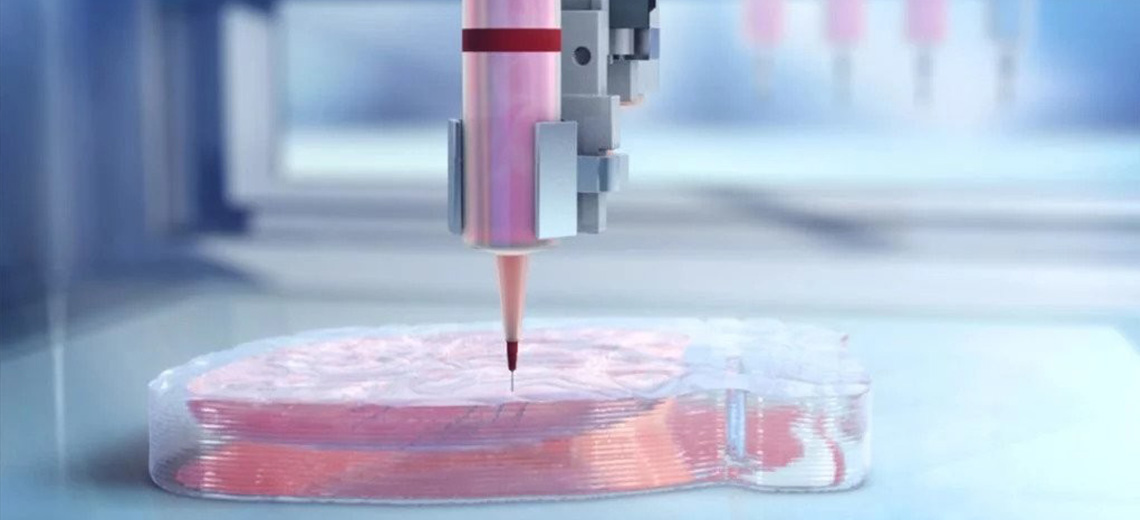
Recent advances in 3D printing, which uses biomaterials, biomolecules, and/or cells, have given scientists unprecedented capacity for developing tissue-engineered constructs with complex 3D geometries such as heart valves.

Composite inks were formulated from synthetic and natural polymers, namely poly(vinyl alcohol) (PVA), gelatin, and 𝜅-carrageenan. PVA is characterized by water solubility, biocompatibility, mechanical properties, and biodegradability. Besides, PVA can be physically crosslinked and create PVA-based cryogels through cyclic freeze-thawing steps, this feature eliminates the use of potential cytotoxic chemical crosslinking agents. Gelatin is a polypeptide largely used in developing tissue engineered scaffolds to promote bioactivity, biocompatibility, and bioresorption. Finally, 𝜅-carrageenan is a polysaccharide that is capable of producing thermosensitive hydrogels through helix formation. Its functional groups, including sulfate and hydroxyl groups, could also enhance interactions and bonding between these three components. These characteristics make it a promising rheological modifier for 3D printing purposes.
Various compositions were investigated to find the printable inks. Moreover, comprehensive physicochemical, structural, mechanical, rheological, and biological properties of developed constructs were evaluated.
The mechanical properties were shown to be comparable to the native valve leaflets: the hydrogels are capable of withstanding cyclic compressions with similar frequencies to a native heart (i.e., 1 Hz). From the biological point of view, composite scaffolds revealed high biocompatibility assessed by in vitro cell culture using inhabitant valvular cells (VICs). From the structural point of view, VICs showed expected fibroblastic phenotype with the expected morphology. In vitro hemocompatibility assessments have proved minimal hemolysis of the proposed hydrogels with low thrombogenicity. Furthermore, subcutaneous implantation showed that fabricated hydrogels induced a nonchronic inflammation response and underwent in vivo resorption and remodeling, reconfirming the biocompatibility of the hydrogels in physiological conditions.
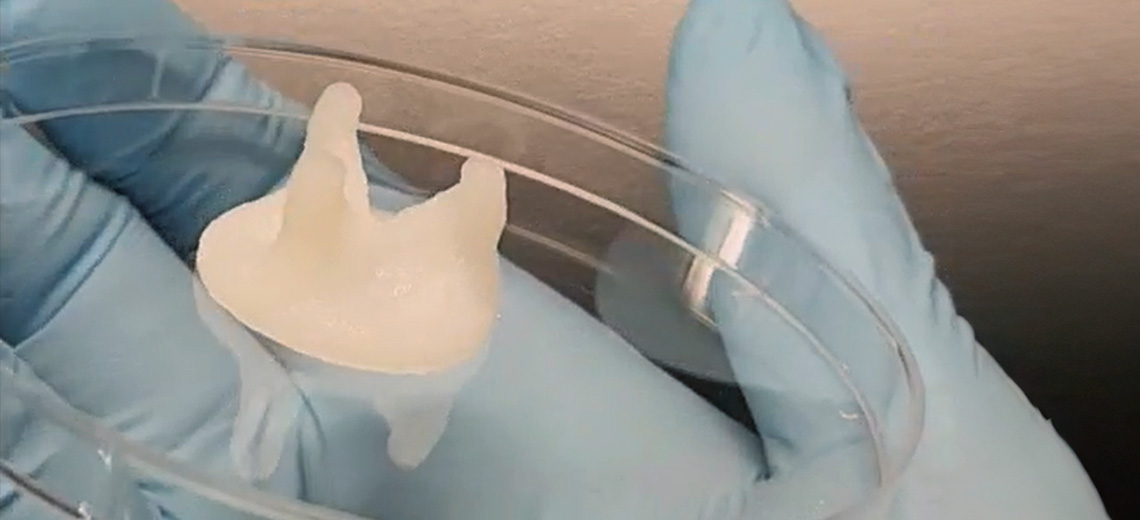
From the printability assessment conducted, it was found that the P10/G2.5/C2.5 ink exhibited the most suitable rheological properties and is best suited for 3D printing. Therefore, it has been selected for the 3D printing of a tricuspid heart valve without the need for support structures or baths.
Printability assessment and printing of the heart valves were performed using a BIO X6 bioprinter (CELLINK, USA). For this purpose, the inks were loaded into 3 mL cartridges fitted with 25G blunt needles and cooled to 25 °C before extruding. The printing was performed at 25 °C with a 25G blunt needles nozzle, nozzle movement speed of 5 mm s−1, 25% infill density with rectilinear infill pattern, and printbed temperature set at 4 °C.
Heart valves of 25 and 13 mm in diameter have been printed and the printed constructs showed successful printing of valve leaflets and sinus of Valsalva, confirming the possibility of printing heart valves that contain features and details observed in the native tissue.

Moreover, bioprosthetic-like valves have been printed with a diameter of 27 mm, which is close to the size of a native valve. After crosslinking using the freeze-thawing cycles, the valves were easy to manipulate and hold with a hand, and the leaflets were pliable and flexible.

The preliminary evaluation of the function and integrity of the 3D-printed heart valves under physiological conditions was performed using a custom-made pulse duplicator system.
The 3D-printed pediatric-sized tri-leaflet valve has been tested under 90 BPM frequency (pediatric condition). The valve leaflets opened and closed properly, with complete leaflet coaptation during each cycle. In systole, the pressure increases in the left ventricle and exceeds the aortic pressure, leading to the opening of the valve leaflets and the ejection of the fluid. Next, when the aortic pressures become higher than the ventricular side, during diastole, the aortic valve will close. The maximum opening area was calculated to be ≈16%. The peak-to-peak pressure gradient, extracted from the recorded pressure waveforms, was 31 mmHg, suggesting a mild stenotic behavior of the aortic valve. This could be attributed to the mismatch between the valve size and the aorta model or to the digital design of the valve.

The larger (27 mm diameter) bioprosthetic like valve was tested using a 70 BPM frequency to simulate adult physiological conditions. The valve demonstrated appropriate opening during systole and complete closing during diastole, with a larger maximum opening area of ≈33%. On the other hand, compared to the other valve, the peak-to-peak transvalvular pressure gradient was less than 13 mmHg.

3D printing of heart valves faithful to the structure of native ones has yielded more than decent results. Future steps will involve improving CAD designs, printing new valves, and thoroughly studying the efficiency of manufactured valves in vitro under physiologically relevant pulsatile flows. Ultimately, the valves should be implanted as substitutes in an animal model to assess functionality in vivo.
These technologies aim to offer personalized and durable solutions for patients with heart diseases, paving the way for a future where medical treatments are increasingly tailored to individual needs and patient health.
Source: Wiley online library